Frozen Shoulder: Do I need a steroid injection?
Frozen Shoulder: Do I need a steroid injection?
Tommy Conway, Chartered Physiotherapist and Director at OneHEALTH, Physiotherapy Clinic Tullamore.
Are you struggling to lie on your shoulder at night? Struggling to reach back for the seat belt? Struggling to reach overhead? Have you noticed you are starting to lose movement in your arm? Has it slowly gotten worse and worse? Have you been told you have a frozen shoulder and more importantly have you been told you need a steroid injection. I am writing this article not to discredit a steroid injection but through my clinical experience people simply get the steroid injection at the wrong time. Also, the most common question that is asked is why? Why has this happened to me? And why now? There are certain arguments to how a frozen shoulder can happen, for example not doing enough overhead activities but I have seen clients with frozen shoulders who’s professions are reaching overhead, Painters and plasterers. Another argument is that they have weak shoulders and people don’t spend enough time bearing weight on their shoulders. Well, if that was the case then why don’t we get frozen knees, hips and ankles? There are a lot more theories to why it happens but not enough concrete evidence to indicate a direct cause, it’s a mystery, but that doesn’t mean we can’t intervene and get a positive outcome. You have to intervene with the right interventions at the right time and most people don’t. Believe me they don’t and that’s why I am writing this article.
What is Frozen shoulder?
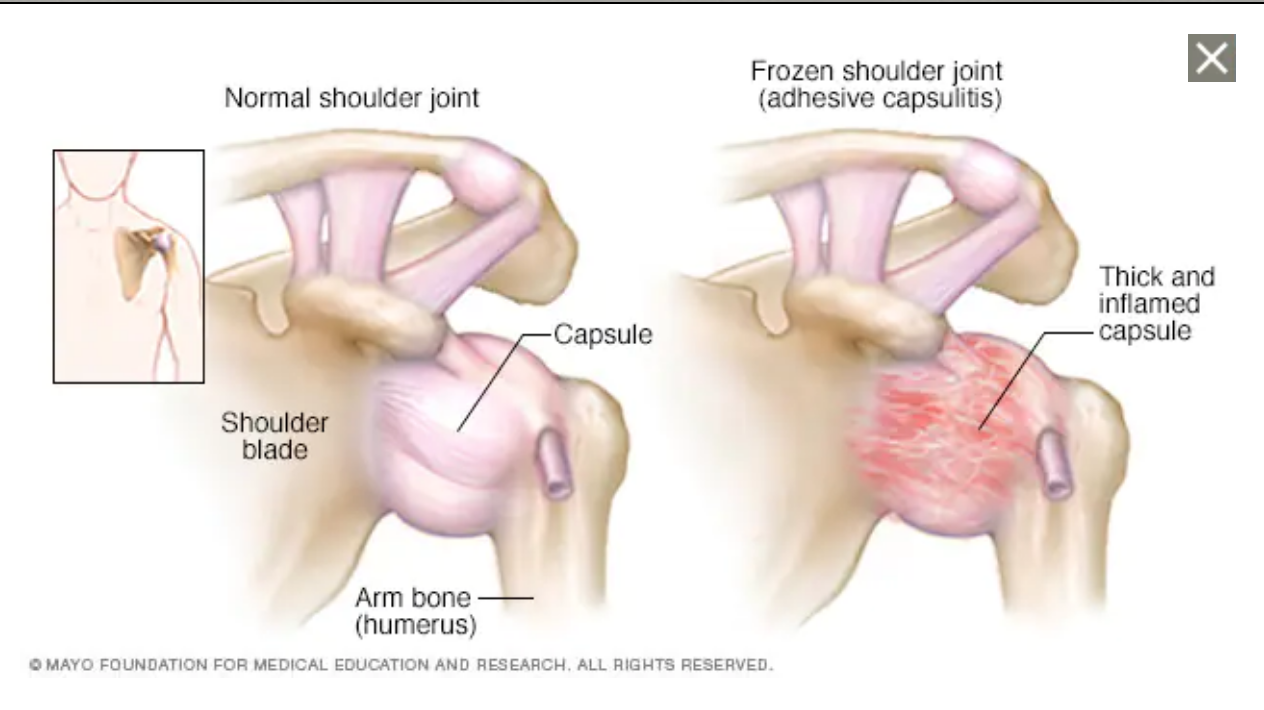
Frozen shoulder is also known as adhesive capsulitis, it is an inflammation of the capsule of the shoulder. This is a very painful condition, with a severe loss of shoulder function and movement. This is a slow process to get better, it can take up to 9 months but some people suffer for years. The key to getting this condition better, is detailed diagnosis and timing the intervention correctly.
The shoulder comprises three bones, the collar bone, scapula (Shoulder blade) and the arm (Humerus). Where the arm bone connects in the shoulder blade is called the Glenohumeral joint and this is where your capsule is. The Capsule of the shoulder comprises ligaments and a labrum, these structures are designed to prevent the shoulder from moving out of place, they are deep and robustly strong structures. If this structure is torn, your shoulder can regularly dislocate. Do you remember in the film lethal weapon where Mel Gibson’s character kept dislocating his shoulder? That’s because he had a torn labrum. This torn labrum makes the glenohumeral joint very loose and easy to move, that is the direct opposite of Adhesive Capsulitis (Frozen shoulder), It becomes stiff and hard to move.
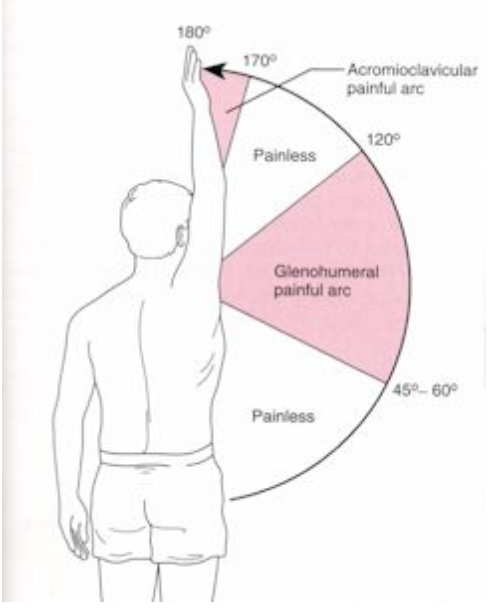
The glenohumeral joint has 60 degrees of movement, as you can see in the picture there is a total of 180 degrees of shoulder movement. The glenohumeral joint (Capsule) only makes up one third of the movement, but the standard presentation of a frozen shoulder is a far greater loss 120 - 180 degrees. So, are we missing something? Where does the remaining 120 degrees movement come from and can we get that back?
This is how you make up 180 degrees of movement in the shoulder.
- 60 degrees: glenohumeral joint
- 60 degrees: Scapula upward rotation
- 60 degrees: rib cage movement
Where are all the traditional interventions focused on
- Steroid injection: glenohumeral joint
- Anti-inflammatories: glenohumeral joint
- Physiotherapy stretches: glenohumeral joint.

The first two interventions are designed around getting the capsule to relax the inflammatory process at the glenohumeral joint which should allow for greater pain relief and movement. The problem is we are focusing all our efforts on 60 degrees of movement when maybe it is not ready to relax and loosen, what about the other 120 degrees? This is why timing and knowing when to intervene becomes the skill. When examining my clients, I can identify how much movement is in the glenohumeral joint, scapula, and ribcage. This gives me an idea of what intervention to start with. For example, I have three different client scenarios.
1: Client with 40 degrees of movement at the glenohumeral joint and 0 degrees at the scapula and rib cage. My intervention will be to do hands on treatment and exercise to restore the scapula movement and rib movement. I will not be advising a steroid injection because it is not the glenohumeral joint that is causing the loss in movement.
2: Client with 0 degrees of movement at the glenohumeral joint and 60 degrees at the scapula and a further 30 degrees at the ribcage. I will first restore the rib cage movement first and then refer for a steroid injection to help restore the glenohumeral joint movement.
3: Client with 0 degrees of movement at the glenohumeral joint, 0 at the scapula and 0 at the ribcage. This client is very stuck but timing is important here. I would spend 6 - 12 weeks restoring movement in the scapula and rib cage and then I would refer for a steroid injection to help with the glenohumeral joint.
The question that is on the tip of your tongue is, “should I get a steroid injection?” The answer is a simple one. For the steroid to have a beneficial effect you need the other factors to be moving better first. You need more than a diagnosis, you need to understand how well the glenohumeral joint is moving? How well the scapula is moving? And how well the ribcage is moving? Then and only then can you make the right intervention at the right time.
Thanks for reading and if you have any questions reach out to me at tommy@onehealth.ie
Tommy.


